The Sioux Lookout First Nations Health Authority’s (SLFNHA) held its two-day annual general meeting last week. It serves 33 First Nations — 28 of them are considered remote as they have no highway access.
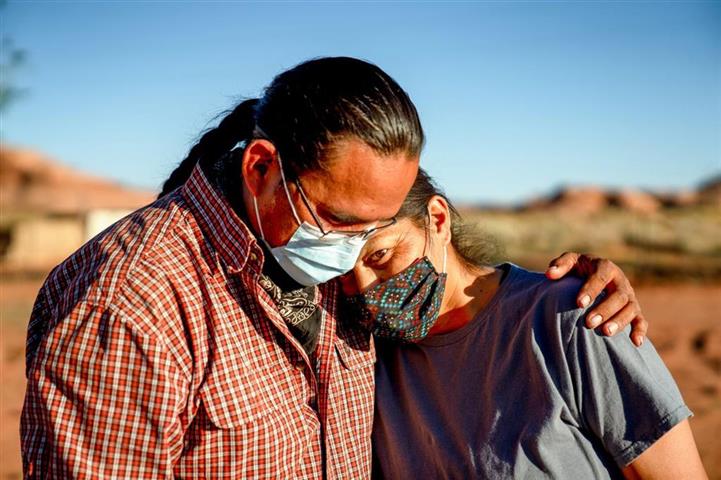
From 2011 to 2021, emergency department visits for intentional self-injury nearly doubled and ambulatory visits in the communities tripled.
The steering committee involved in SLFNHA’s mental health report has been listening to stories from community members to integrate Indigenous knowledge into its findings, Dr. Lloyd Douglas, SLFNHA’s public health physician, stated.
“When you hear the storytellers sharing their experiences, you quickly realize that each statistic, each number, is a person, is a mom, is a dad, is an aunt, an uncle, a cousin,” Douglas said. “This is not something that’s historical — this is extremely current.”
While much of the data gathered goes up to 2021, he suspects the numbers have worsened since then.
It’s hoped the final report will be completed by November, in time to be presented at a special meeting of chiefs. The goal of the report is to provide First Nations people with quantitative evidence that can be used to push for more resources.
“It will validate their stories,” Douglas said. “Their voices will be amplified through this report.”
Several new projects have been implemented in Sioux Lookout, which acts as a hub for surrounding First Nations to access health care and social services to meet people’s mental health and addictions needs.
These include the opening of safe rooms at the Meno Ya Win Health Centre, a new walk-in addictions clinic at both the hospital and emergency shelter, and new supportive treatment beds.
SLFNHA also purchased a third hostel this spring to help accommodate some of the thousands of people who go to the town for medical appointments.
“From the perspective of a co-ordinated continuum of care, it’s important to have a suite of services,” said Sonia Isaac-Mann, the SLFNHA’s chief executive officer and president.
“Those wraparound services that are needed so [they] don’t just go into treatment — there’s more to it than that, and it’s looking at: how do we support them on their journey to healing and wellness?” she said.
Isaac-Mann said she sees SLFNHA’s role as helping to co-ordinate different partners. She supports the chiefs’ mental health resolution, and hopes to work closely with communities and organizations to help them achieve their goals.
“[The resolution] is very timely and it really puts everybody who has a role to play in this system on alert that we need to do this work, we need to do it now, it’s not three years from now.”
SLFNHA is finalizing a new mental health model for the First Nations it serves. Chief operating officer Janet Gordon said the framework takes into consideration a comprehensive mental health and addictions review, and community consultations.
“We need a long-term solution and we need … infrastructure to support that at the community level,” Gordon said. “It’s developing those business plans, developing work plans with the communities, with different groups, and putting some timelines around it.”
“We have identified a model that could address some of those areas in terms of being able to better respond to individual needs so that they can have access to service,” she said. “Doing more prevention and promotion so we’re not waiting for people to be in crisis or that they are not taking their own lives.”
Another key focus is providing care to youth, and ensuring they have safe spaces in their communities and are empowered to lead the next generations, Gordon said.
pll/mem/adr